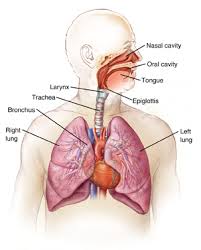
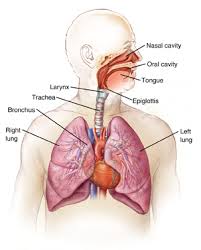
Understanding pneumonia is easier when you understand the respiratory system. Respiration is the process by which humans take in oxygen and remove carbon dioxide. The respiratory system is composed of the nasal passage, the pharynx, larynx, the trachea, bronchi and lungs.
When you inhale air through your mouth or nose, your diaphragm tightens and moves downward which enlarges the chest cavity. The air you just inhaled travels down your windpipe and into your lungs passing through the main airways called the bronchial tubes. The air then reaches the air sacs called alveoli located at the end of the bronchioles. The air then passes through the thin walls of the alveoli to the capillaries, which are very small veins. Hemoglobin (a protein found in red blood cells) helps to move oxygen from the alveoli to the blood. The pulmonary vein carries this oxygen-rich blood from the lungs to the left side of the heart. The left side of the heart pumps the blood to the rest of the body.
When you exhale the diaphragm does the opposite as it did when you inhaled: it relaxes and moves upward reducing the chest cavity, and forcing the waste product carbon dioxide out of your lungs and then out of your mouth or nose.
Pneumonia
Pneumonia is a lung inflammation that occurs when bacteria, a virus, or chemicals are inhaled into one or both lungs. Infection can also occur following an infection in the bloodstream, or after trauma or surgery in or near the lungs. When the immune system tries to fight these organisms, the lungs’ air sacs become inflamed and filled with fluid, making it difficult to breathe.
Types of Pneumonia
There are four types of pneumonia:
Community-acquired pneumonia (CAP) is the most common type of pneumonia. As the name suggests, most people catch it in public areas such as work, school or the grocery store. Sixty percent of CAP cases are caused by a bacteria called Streptococcus pneumonia and is treated with antibiotics.
Hospital-acquired pneumonia is a type of pneumonia that is caught while one is staying in the hospital or nursing home, and especially if in an intensive care unit (ICU) or if using a ventilator to help breathe. Hospital-acquired pneumonia can be very dangerous, especially for young children, older adults and people who have weakened immune systems. It’s generally treated with antibiotics, often given intravenously while in the hospital.
Aspiration pneumonia is a type of pneumonia that develops after particles are inhaled into the lungs. This occurs when small particles enter the lungs after vomiting, or in older patients or stroke victims with poor swallowing mechanisms when they inhale the acidic contents of their stomachs. This can cause inflammation, which can lead to a bacterial infection that is treated with antibiotics.
Opportunistic pneumonia is a type of pneumonia that affects people who have weakened immune systems, particularly those with human immunodeficiency virus (HIV), acquired immunodeficiency syndrome (AIDS), chronic obstructive pulmonary disease (COPD) or people who have recently had an organ transplant.
Symptoms of pneumonia
The symptoms depend on the type of pneumonia; with some kinds of pneumonia not having symptoms at all. In general, symptoms tend to mimic those of a cold or the flu and can include: Cough, often accompanied by green, yellow, or sometimes bloody phlegm
Fever with or without chills
Sharp chest pain that gets worse with deep breathing or coughing
Shortness of breath
Fatigue
Shaking chills or persistent fever
Headache
Sore throat
Loss of appetite
Confusion (especially in the elderly)
Who is likely to develop pneumonia?
Pneumonia can occur in people of all ages, but it is most common in young children and people older than age 65. The following factors can increase the risk of developing pneumonia:
- Chronic illnesses such as cardiovascular disease and diabetes
- Smoking cigarettes
- Abusing alcohol
- Lowered immunity, caused by HIV/AIDS, chemotherapy, or certain drugs
- Being bedridden, unconscious for along period, or paralyzed.
- Exposure to certain pollutants or potentially toxic chemicals
Diagnosis
A doctor may suspect pneumonia if they hear crackling and wheezing sounds when listening to a patient’s lungs. A chest x-ray will usually confirm the presence of fluid in the lungs that indicates pneumonia. Sometimes additional tests are performed, including blood tests and cultures of lung fluid or sputum.
Medical Treatment
Conventional treatment for bacterial pneumonia is likely antibiotics. These medications won’t help for viral pneumonia, and treatment is similar to that for the flu – rest and fluids – although antiviral medications can sometimes help. A doctor may recommend over-the-counter drugs that can ease pain and relieve fever. Severe pneumonia requires treatment with intravenous medications, and with sometimes supplemental oxygen is necessary.
Other aspects of Healing
Breathing warm, moist air may help to loosen the sticky mucus in your lungs.
Place a warm, wet washcloth loosely over your nose and mouth and breathe normally.
Use a humidifier with warm water and breathe in the warm mist.
Take a couple of deep breaths two times an hour, which will help open your lungs.
While lying down, tap your chest gently a few times a day, which helps bring up mucus from the lungs so that you can cough it out.
Staying well hydrated. Fluids can help loosen the mucus in your lungs. Good choices are water, warm tea and clear soups. Many believe that dairy products increase phlegm production, so if you find that drinking dairy milk worsens your symptoms, drink nut milk, coconut milk or rice milk instead.
Avoid alcohol and highly caffeinated drinks, such as energy drinks and coffee, which can interfere with rest.Do not smoke and do not expose yourself to secondhand smoke. Avoid breathing in toxic fumes of any kind and if you must be around them, wear a protective mask.
 Movement is good for your whole body and especially your lungs. Exercise makes your lungs stronger and better at giving your body the oxygen it needs, which also helps your immune system. Heal and then begin regular movement.
Movement is good for your whole body and especially your lungs. Exercise makes your lungs stronger and better at giving your body the oxygen it needs, which also helps your immune system. Heal and then begin regular movement.